|
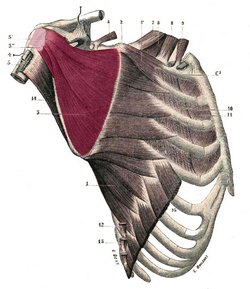
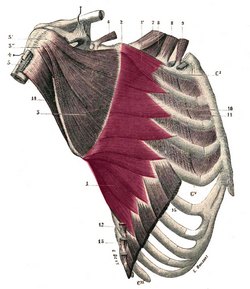
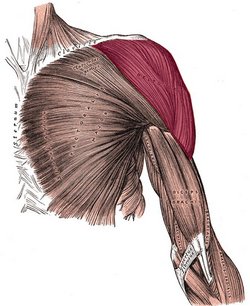
The deltoid or deltoideus (Latin) is a large, thick, triangular muscle, which covers the glenohumeral joint anteriorly, superiorly, and posteriorly. It can be described as having three components or segments, anterior, middle, and posterior. The anterior portion originates from the lateral third of the clavicle, on the clavicle’s superior border. The middle portion originates from the lateral border of the scapula’s acromion, and the posterior portion originates from the spine of the scapula. All three portions insert laterally by means of a thick tendon on the deltoid tuberosity of the humerus. At its insertion the muscle gives off an thick connective tissue expansion to the deep fascia of the arm.
The three portions of the deltoid muscle are usually well defined. As an anatomical variation, the clavicular or the acromial portion of the muscle may be absent.
This muscle is innervated by the axillary nerve (C5, C6), a branch of the brachial plexus, and supplied by the posterior circumflex humeral artery and the deltoid branch of the thoracoacromial artery.
The word deltoid is derivates from the Greek word [δελτοειδής] which is itself formed by the terms [δέλτα] (délta), referring to the triangular shape of the letter delta (uppercase Δ, lowercase δ) and [-οειδής] (-oeidís), a the Greek suffix meaning “similar to”. Delt-oid then would mean “similar to a Δ (delta)".
The deltoid is one of the 17 muscles that attach to the scapula.
|
Deltoid muscle.
Click on the image for a larger depiction |