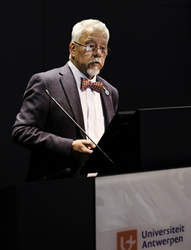
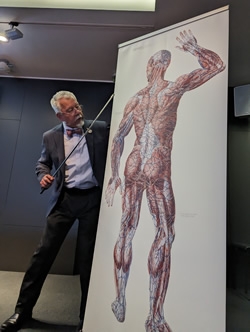
Dr. Miranda speaking at the
2023 Vesalius Triennial
I had the honor of being invited by the University of Antwerp in Belgium to speak at the 2023 Vesalius Triennial Meeting in the city of Antwerp. This scientific meeting was presented in conjunction with the 29th Congress of the Association Européenne des Illustrateurs Médicaux et Scientifiques - AEIMS (European Association of Medical and Scientific Illustrators). A three-day program that, alongside the scientific program, included poetry, art, music, sculpture, and painting. All of this celebrating the life and inspiration brought to arts and medical science by Andreas Vesalius Bruxellensis (1514-1564).
The scientific program included lectures by well-known Vesalius scholars, including Vivian Nutton, Robrecht Van Hee, Francis Van Glabbeek, Philip Van Kerrebroeck, Omer Steeno, Maurits Beisbrouck, Theodor Godeeris, Peter Bols, and many others. Personally, it was incredible to be invited to this event and share with these individuals.
One of the events of this meeting was an afternoon concert entitled “Vesalian landscapes in music, poetry, and photographs” by pianist Elke Robersscheuten, and my friend Theo Dirix, who read the poetry. This was accompanied by slides of Vesalian works, and images of the city of Brussels and the island of Zakynthos, Greece. One of the pieces performed by Elke Robersscheuten was “André Vésale”. Ths rare piece of piano sheet music is the topic for a separate article in this blog: An anatomical surprise from a French composer.
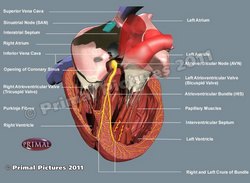
My presentation was entitled “Vesalius and Anatomical Megadrawings – A Personal Journey”. This is a topic that touched on my experience with larger (and very small) books and the sentence written by Andreas Vesalius in the two-page letter to Johannes Oporinus printed in the first part of Vesalius’ opus magnum “De Humani Corporis Fabrica, Libri Septem”. Referring to anatomical images, Vesalius states “quod tabulas quæe nunquam satis magna studiosis proponi poterunt”. Daniel H. Garrison in the latest publication of the Fabrica translates this as “illustrations which could never be large enough for students”.
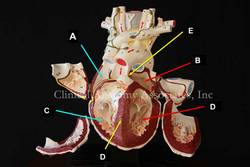
The need for better resolution and the limitation of the printing technology (hand-carved woodblocks) at the time as well as the quality of the paper available forced the need for larger images. The Fabrica is a folio-size book and the images for the first time are labeled with letters, symbols, and characters with a detailed key as to their meaning.
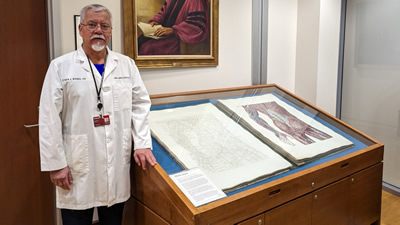
The research for this presentation took me to the largest anatomy book ever printed, the “Anatomiæ Universæ Icones” by Giovanni Paolo Mascagni (1755 – 1815), a double elephant folio size book measuring 40 by 30 inches with two sets of 44 plates. This book was printed in black and white and hand-colored by Antonio Serantoni (1780 – 1837), an Italian engraver and painter. The printing and coloring of this book took ten years between 1823 and 1832. An incredible book of which there are 16 known copies in the world, one of them at the University of Cincinnati.
Anatomiæ Universæ Icones by Paolo Mascagni at the University of Cincinnati
One of the most interesting aspects of this book, besides the large size of each image, is the fact that a 5.9 feet tall human can be constructed if three pages are cut and placed together. Of course, this cannot be done with these incredibly rare and expensive books; but digital technology allows us to scan and lightly correct the background to eliminate imperfections and damage caused by 200 years of use.
With the help of the University of Cincinnati authorities, Gino Pasi (archivist and curator of the Henry R. Winkler Center for the History of the Health Professions at UC), and Samantha Scheck (graphic designer) we were able to access the Mascagni book, measure the images, scan them, and them digitally process them. The result were two large images that I took to Antwerp, receiving incredible feedback from the attendees.
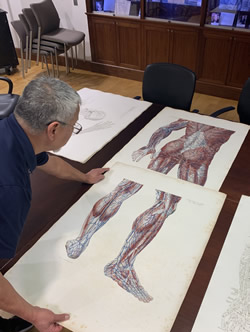
Working with the Mascagni book
The life-size anatomy imagined by Mascagni
There is so much more to the life of Paolo Mascagni, before and after his death that include prison, family problems, greed, plagiarism, and a separate individual that is now known for his “dubious character”. I will write separate articles on these topics.
My presentation also touched on the large poster-like drawings (not books) that were used for anatomical teaching before the advent of the 35 mm slide projector and later PowerPoint with halogen light bulb projectors and today large LED monitors.
The anatomy amphitheater at the University of Chile Medical School
3 by 4 feet scroll painting by Juan Frutos M.
My alma mater, the University of Chile Medical School,has a museum and an old wooden amphitheater where I studied anatomy many years ago. As seen in the accompanying image, this auditorium has two incredibly large hand-drawn images that measure 13 feet in height and 5 feet in width.They are copies of the "Traité complet de l’anatomie de l’homme"
by J.M. Bourgery (1831-1854) made by the Chilean painter Juan Frutos M.
The anatomy amphitheater has been deemed National Heritage by the government of Chile and it will be preserved as is. Below the seating area there was a room closed for decades. In it there were found 500 large scrolls that are worthy of research and preservation. These were hand-painted by 47 different authors, some medical students and artists. From the artistic point of view, research needs to be done on the media used as well as the method of painting.
In the time I was a student, these scroll megadrawings were not in use as an old electric arc projector with glass slides were used in its place.
The information on these drawings can be found in the book “Instituto de Anatomía: Un Recorrido Visual” by Prof. Julio Cárdenas V. My personal thanks to Dr. Cárdenas for facilitating digital images of his book for my presentation.
The meeting included an artistic midday soiree entitled “Vesalian Landscapes in music, poetry and photographs” by pianist Elke Robersscheuten and Vesalius expert and taphophile Theo Dirix.
This afternoon concert was followed by scientific poster presentations, an exhibit of anatomical art, and presentation of art and medical books, including “The King’s Anatomist” by my friend Ron Blumenfeld.
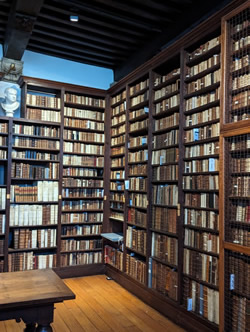
As the closure of the meeting, the attendees were invited to a guided tour of the Plantin-Moretus Museum, an institution that preserves the rich history of printing in the 16th century. This tour also deserves a separate article with pictures.
Francis Van Glabbeek, an orthopedic surgeon at the University of Antwerp invited my good friend Dr. Randall Wolf and me to visit his personal rare book collection, which includes not only a 1543 and a 1555 Fabrica, but rarities like books by Bidloo, Cowper, Hyeronimus Fabricio de Aquapendente, and a copy of the “Epistola rationem modumque propinandi radicis Chynae decocti” which was one of the books mentioned in my presentation. A meeting that only collectors of rare books could understand! Later in the day Dr. Van Glabbeek took us to Verrebroek, the city where another famous Flemish anatomist was born: Philippo Verheyen.
Admiring the title page of the 1543 Fabrica
Dr. Van Glabbeek and the statue of Philippo Verheyen
Comparing 1543 and 155 editions
The Plantin-Moretus Museum
I cannot end this article without reiterating my thanks for the invitation to the organizing committee of this fantastic meeting:
Ann Van de Velde
President AEIMS, University of Antwerp
Pascale Pollier-Green
Past-president AEIMS, University of Antwerp
Francis Van Glabbeek
President BIOMAB, University of Antwerp
Bob Van Hee
Emeritus Professor of Surgery and Medical History
Director of the Lambotte Museum for the History of Health Care, University of Antwerp
Marc de Roeck
University of Antwerp
PERSONAL NOTE: I was invited to deliver a variation of this presentation in November 2023, at the LVIII Chilean Anatomical Society Meeting in Santiago, Chile.