|
The mandibular canal is a long, bilateral canal which runs along and within the mandible. This canal transports the inferior alveolar neurovascular bundle. The mandible is known vernacularly as the “jawbone” or “lower jaw”.
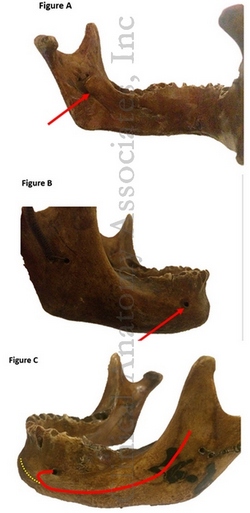
The mandibular canal starts on the medial surface of the mandibular ramus at the mandibular foramen (Figure A, arrow) descends anteroinferiorly through the body of the mandible until it ends in the mental foramen at the buccal (anterior) surface of the mandible, usually in the area between the premolars (Figure B, arrow).
Before exiting, the canal forms an “anterior loop” projected anterior to the mental foramen prior to changing its direction back and outwards in direction to the buccal plate (Figure C, red line). This last portion of the canal is called the “mental canal”.
A frequent anatomical variation is the presence of a bifid mandibular canal (recent studies indicate it has a prevalence of around 16%).
Different anatomical studies show that the mandibular canal not only finishes at the mental foramen, but it could divide itself giving an incisive canal which runs anteriorly onto the incisal region (Figure C, yellow line). When it doesn’t continue as an incisal canal, the neurovascular elements go anteriorly through the cells of the spongy bone tissue.
The presence of this Incisal canal has surgical relevance, and knowledge of its exact location and anatomical parameters has a high importance on reducing complications of surgical procedures in the mental area such as dental implants, bone lesions removal and bone harvesting among others, all which could damage the incisal canal and the neurovascular bundle inside it.
With the latest use of CBCT (Cone Beam Computed Tomography) technology to evaluate anatomical structures, the presence of this canal has showed to be high (92-100%) and its length can vary from reaching only the premolar area or even the central mandibular incisors in the least of cases.
|